INTRODUCTION
Sepsis is a life-threatening condition resulting from a dysregulated host response to infection, ultimately leading to organ dysfunction. It is recognized as a global health priority, with the World Health Organization (WHO) estimating that sepsis affects approximately 49 million people each year and contributes to 11 million deaths. This represents nearly one in five global deaths annually1. Despite being preventable and treatable in many cases, sepsis remains one of the most underrecognized and underreported health threats, especially in low and middle-income countries (LMICs), where nearly 80% of the cases occur1,2.
Sepsis disproportionately affects individuals with underlying health conditions such as diabetes, cardiovascular disease and immunosuppression. Common sources of infection leading to sepsis include respiratory tract infections, urinary tract infections, abdominal infections, and skin or soft tissue infections2,3. The predominant microbial agents vary between regions. Usually, gram-positive bacteria are more frequently identified in high-income settings, while gram-negative organisms dominate in LMICs, although increasing use of invasive medical procedures has begun to shift this distribution4-6.
In Bhutan, there is a significant lack of comprehensive epidemiological data on sepsis, particularly among the adult population. Existing studies are limited, focusing primarily on neonatal sepsis, where gram-negative organisms were identified as the predominant pathogens7. This lack of data represents a critical gap in understanding the burden, clinical characteristics, and outcomes of sepsis in the Bhutanese adult population. Therefore, this study aims to address this gap by determining the mortality rate and clinical profile of patients with sepsis admitted to Department of Medicine at the Jigme Dorji Wangchuck National Referral Hospital (JDWNRH).
METHODS
Study Design
A cross-sectional study was conducted in the Department of Medicine at the JDWNRH in Thimphu, Bhutan. It was conducted over a year long period, spanning 1st January 2021 to 31st December 2021.
Study setting
The JDWNRH, located in Thimphu is Bhutan's tertiary care center and functions as a teaching hospital. It offers a comprehensive range of services, which includes emergency care, inpatient and outpatient services, specialized clinics, and rehabilitative care. The hospital houses departments such as Medicine, Surgery, Paediatrics, Obstetrics and Gynaecology, Psychiatry, and others.
In 2021, the Department of Medicine had 36 in-patient medical beds and medical out-patient clinics (OPD) that operated six times a week. The Intensive Care Unit (ICU) had 10 beds, and the High Dependency Unit (HDU) had 4 beds. The department was staffed by a multidisciplinary team including 15 consultants, 10 internal medicine residents and 42 nurses.
Study participants
All patients with sepsis admitted to the Department of Medicine at the JDWNRH were eligible participants.
Inclusion Criteria: All patients >18 years diagnosed with sepsis based on the System Inflammatory Response Syndrome (SIRS) and quick Sequential Organ Failure Assessment (qSOFA) criteria.
SIRS criteria: At least two of the following four criteria must be present to diagnose sepsis: temperature <36 °C or > 38 °C; heart rate >90/min; respiratory rate >20/min; white blood cell (WBC) count < 4000 cells/mm3 or > 12000 cells/mm3 or > 10% immature band forms8.
qSOFA criteria: At least two of the following three criteria must be present for sepsis and it indicates organ dysfunction: systolic BP <100 mmHg; respiratory rate >22/min; altered mental status characterised by GCS <159.
Exclusion Criteria: Post-operative sepsis, surgical site infections and cases without consent.
Sample size calculation
In 2017, 544 cases of sepsis were recorded among patients aged 15 and above in Bhutan10. Data from JDWNRH was not available. A 50% prevalence was assumed for the study using the equation [Np (1-p)]/ [(d2/Z21-α/2*(N-1)+p*(1-p)] available online (OpenEpi.com). The following inputs were utilised: hypothesized % frequency of outcome factor in the population (p) of 50%; population size (for finite population correction factor fpc) of 544; confidence limits as % of 100 (absolute +/-) (d) of 5% and the design effect of 1. The sample size (n) obtained was 241 at 95% confidence interval.
Sampling method
A convenience sampling method was used to include all patients with sepsis meeting the inclusion criteria.
Study variables
Sociodemographic variables (age and sex), underlying co-morbidities (chronic kidney disease, diabetes mellitus, hypertension, heart disease, malignancy, chronic obstructive pulmonary disease, etc…), causes of infections (gram positive, gram negative, others), and outcome of the patient (alive or dead) were collected for the study.
Study tool
A structured interviewer-administered research questionnaire was used for collecting the data.
Data Management
The nurses of the Medicine Ward were trained as data collectors. They were trained on the study instrument, consent form, and the data collection procedure. The collected data were checked for completeness daily by the investigator to monitor the overall quality of the data collection process. Completed questionnaires were stored under lock and key by the investigator.
Data Analysis
The demographic and clinical data collected via the paper-based questionnaire was later securely digitized in EpiData (version 3.1, EpiData Association, Odense, Denmark) software with double data entry to minimize errors. Statistical analysis was conducted using EpiData Analysis (version 2.2.2.183, EpiData Association, Odense, Denmark). The adjusted analysis was done using STATA (version 12.1, copyright 1985–2011 StataCorp LP USA, serial number: 30120504773). Descriptive statistics were used to summarize patients’ clinical characteristics, microbiological profile and outcomes. Chi-square test was used to identify associations between independent variables and mortality with a p-value < 0.05 being considered statistically significant. Binary logistic regression was used to calculate crude odds ratio and adjusted odds ratio to estimate the strength of association between potential risk factors and mortality.
Ethical Considerations
Ethical clearance was obtained from the Interim Institutional Review Board (INTERM IRB/P020/015/449), Khesar Gyalpo University of Medical Sciences of Bhutan. Informed written consent was obtained from eligible participants or their primary guardian, after they received detailed information about the study's purpose, procedures, risks, and benefits. Participation was voluntary, with the option to withdraw without affecting medical care. Patients were anonymized using unique identification numbers. Data confidentiality and protection were maintained, and the study concluded either at patient discharge or upon death.
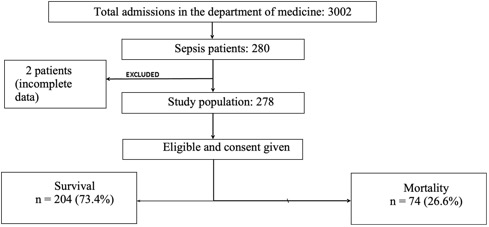
Figure 1. Patients with sepsis at the Department of Medicine, Jigme Dorji Wangchuck National Referral Hospital, 2021
RESULTS
Of the 3002 patients admitted to the Department of Medicine at JDWNRH, there were 278 patients with sepsis. Amongst them, 74 (26.6%) died during hospitalization (Figure 1). As shown in Table 1, more than half (52.1%, 145) were female; and most of the patients with sepsis were aged over 60 years (38.5%).
Hypertension was the most prevalent comorbidity, present in 33.1% of patients, followed by autoimmune diseases, stroke, neurological disorders, HIV and immunosuppressed states collectively accounting for 18.8%, and diabetes mellitus observed in 15.5% of patients (Table 2). As shown in Table 2, pneumonia was the most common source of sepsis (39.2%), followed by urinary tract infections (12.6%) and meningoencephalitis (9.0%). The study revealed that 78.1% of patients required intensive care measures, 24.8% required mechanical ventilation and 53.2% required pressor support.
As shown in Table 3, gram-negative bacteria were the most frequently identified pathogens, particularly Escherichia coli (34.5%) and Klebsiella species (18.5%), followed by gram-positive Staphylococcus species (12.8%).
Table 1: Profile of patients with sepsis admitted to the Department of Medicine at the National Referral Hospital, 2021
|
|
Total |
Survived |
Died |
|
|
Characteristics |
n(%) |
n(%) |
n(%) |
p-value |
|
Sex |
|
|
|
|
|
Male |
133 (47.8) |
93 (45.6) |
40 (54.1) |
0.266 |
|
Female |
145 (52.2) |
111 (54.4) |
34 (45.9) |
|
|
Age (years) |
|
|
|
|
|
18-40 |
82 (29.5) |
68 (33.3) |
14 (18.9) |
<0.001 |
|
41-60 |
89 (32.0) |
59 (28.9) |
30 (40.5) |
|
|
>60 |
107 (38.5) |
77 (37.7) |
30 (40.5) |
Table 2: Clinical profile of patients with sepsis admitted to the Department of Medicine at the National Referral Hospital, 2021
|
|
Total |
Survived |
Died |
|
|
Characteristics |
n(%) |
n(%) |
n(%) |
p-value |
|
Co-morbidities |
|
|
|
|
|
CKD |
26 (14.4) |
22 (17.5) |
4 (7.3) |
0.244 |
|
COPD |
15 (8.3) |
11 (8.7) |
4 (7.3) |
1.000 |
|
DM |
28 (15.5) |
19 (15.1) |
9 (16.4) |
0.637 |
|
Hypertension |
60 (33.1) |
48 (38.1) |
12 (21.8) |
0.252 |
|
Heart disease |
12 (6.6) |
9 (7.1) |
3 (5.4) |
1.000 |
|
Malignancy |
6 (3.3) |
2 (1.6) |
4 (7.3) |
0.045 |
|
Others |
34 (18.8) |
15 (11.9) |
19 (34.5) |
<0.001 |
|
Causes of sepsis |
|
|
|
|
|
Pneumonia |
109 (39.2) |
83 (40.7) |
26 (35,1) |
0.485 |
|
UTI |
35 (12.6) |
30 (14.7) |
5 (6,8) |
0.118 |
|
Meningo-encephalitis |
25 (9.0) |
19 (9.3) |
6 (8.1) |
0.942 |
|
SBP |
24 (8.6) |
10 (4.9) |
14 (18.9) |
<0.001 |
|
Infective endocarditis |
7 (2.5) |
6 (2.9) |
1 (1.3) |
0.679 |
|
GI sepsis |
12 (4.3) |
10 (4.9) |
2 (2.7) |
0.526 |
|
Line infection |
6 (2.1) |
6 (2.9) |
0 (0.0) |
0.347 |
|
Bloodstream infection |
21 (7.6) |
9 (4.4) |
12 (16.2) |
<0.001 |
|
Skin infection |
8 (2.9) |
3 (1.4) |
5 (6.8) |
0.033 |
|
Others* |
31 (11.1) |
28 (13.7) |
3 (4.1) |
0.029 |
|
Intensive care requirement |
|
|
||
|
Mechanical ventilation |
69 (24.8) |
16 (23.1) |
53 (76.8) |
<0.001 |
|
Pressor requirement |
148 (53.2) |
82 (55.4) |
66 (44.6) |
<0.001 |
CKD: Chronic kidney disease; COPD: Chronic obstructive pulmonary disease; DM: Diabetes mellitus; HIV: Human immunodeficiency virus; UTI: Urinary tract infection; SBP: Spontaneous Bacterial Peritonitis; GI sepsis: gastrointestinal sepsis; *Others include autommune, HIV, organ transplant, patient of immunisuppression
There were no significant sex-based differences in mortality. However, advancing age was associated with higher mortality, wherein patients aged >60 years had significantly worse outcomes compared to those aged 18–40 years (p<0.001). While co-morbidities did not have statistically significant differences between survival and death, specific conditions such as malignancy (p=0.045) were linked to increased mortality (Table 4).
There were no significant sex-based differences in mortality. However, advancing age was associated with higher mortality, wherein patients aged >60 years had significantly worse outcomes compared to those aged 18–40 years (p<0.001). While co-morbidities did not have statistically significant differences between survival and death, specific conditions such as malignancy (p=0.045) were linked to increased mortality (Table 4).
As shown in Table 4, Spontaneous Bacterial Peritonitis (SBP) and bloodstream infections were strongly associated with death (p<0.001), while culture reports showed no statistically significant association with mortality. Intensive care measures were notably linked to poor outcomes, with intubation (76.8% in deaths, p<0.001) and pressor use (p<0.001) being particularly significant.
After adjustment, SBP (adjusted OR 3.85, 95% CI 1.43 - 10.3, p=0.007), bloodstream infections (adjusted OR 3.62, 95% CI 1.25 - 10.5, p=0.018), the need for intubation (adjusted OR 23.5, 95% CI 11.2 - 49.2, p<0.001) and pressor support (adjusted OR 9.78, 95% CI 4.02 - 23.8, p<0.001) remained independent predictors of death (Table 4).
Table 3: Microbiological profile of patients with sepsis admitted to the Department of Medicine at the National Referral Hospital, 2021
|
Characteristics of culture reports |
Total |
Survived |
Died |
|
|
n(%) |
n(%) |
n(%) |
p-value |
|
|
Gram negative bacteria |
|
|
||
|
Acinetobacter |
4 (3.9) |
3 (4.9) |
1(4.0) |
0.576 |
|
Escherichia coli |
36 (34.5) |
10 (16.4) |
6 (24.0) |
0.706 |
|
Klebsiella |
19 (18.5) |
15 (9.2) |
4 (16.0) |
0.419 |
|
Pseudomonas |
12 (11.7) |
8 (13.1) |
4 (16.0) |
0.738 |
|
Gram positive bacteria |
|
|
|
|
|
Staphylococcus |
13 (12.6) |
10 (16.4) |
3 (12.0) |
0.524 |
|
Enterococcus |
5 (4.9) |
4 (6.6) |
1 (4.0) |
0.329 |
|
Streptococcus |
2 (1.9) |
2 (3.3) |
0 (0.0) |
1.000 |
|
Others |
|
|
|
|
|
Tuberculosis |
4 (3.9) |
3 (4.9) |
1 (4.0) |
0.576 |
|
Scrub typhus, Dengue, or Leptospirosis |
8 (7.8) |
6 (9.8) |
2 (8.0) |
0.685 |
DISCUSSION
The study found a notably high in-hospital mortality rate of 26.6% among patients with sepsis admitted to the Department of Medicine at the National Referral Hospital. This underscores the significant burden of sepsis in the country and aligns with mortality rates reported in other low and middle-income countries, which often ranges between 20% and 40% depending on healthcare access, time of intervention, and availability of intensive care facilities4,11,12. Studies in India have reported mortality rates ranging from 51.6% to 65.2%13,14. This finding is particularly significant given that Bhutan provides free healthcare suggesting that high mortality may be attributed more to late presentation, underlying comorbidities, and limited critical care capacity than to economic barriers alone.
Intensive care interventions, specifically intubation (p<0.001) and pressor support (p<0.001), emerged as independent predictors of mortality. A study from Vietnam reported similar results, highlighting that the invasive therapies are often used and offered to critically ill patients with severe sepsis or shock, who already have a low chance of survival15. While these interventions are vital to support and possibly save lives, the underlying fragility of the patients means that the outcomes can often still be poor.
Advancing age is a well-established independent risk for sepsis. Consistent with this, this study found that patients over 60 years experienced significantly higher mortality rates (p<0.001). Similar findings were reported from studies conducted in Bangladesh and Northeast India, where the mean age of patients with sepsis was 55.82 ±19.19 years, with the 61-70 year age group being the most affected11,16. The increased vulnerability of older adults to sepsis is likely attributable to age related immune decline, reduced physiological reserves, and a higher prevalence of comorbidities17,18. These findings underscore the importance of aggressive management of sepsis for elderly patients with sepsis.
This study found that hypertension and diabetes mellitus were the most prevalent comorbidities among patients with sepsis, though neither showed a significant association with mortality. The presence of malignancy and other immunocompromised states was associated with poor outcomes. Malignancy, in particular, was significantly associated with mortality, likely due to immunosuppression and thus, a delayed recognition of infection. These findings align with previous studies suggesting that immunocompromised states, rather than common chronic illnesses such as hypertension or diabetes, are stronger predictors of adverse outcomes in sepsis11,19.
While sex difference was not significantly associated with mortality, a slight female predominance was observed, consistent with global data published in 20201. Females with autoimmune diseases accounted for 18.8% of the sepsis cases, which may partly explain this trend. It is worth highlighting that the scoring system used for sepsis identification does not incorporate sex as a variable. While physiological and biological differences exist between males and females, the scoring criteria primarily focuses on clinical indicators such as heart rate, respiratory rate and blood pressure9,11,20,21. These parameters may be altered during autoimmune disease flares, potentially resulting in the slight female preponderance in this study.
Table 4: Factors associated with mortality in patients with sepsis admitted to the Department of Medicine at the National Referral Hospital, 2021
|
Characteristics |
OR (95% CI) |
p-value |
Adjusted OR (95%CI) |
p-value |
|
Age (>40 vs 18- 40) |
2.14 (1.12 – 4.10) |
0.020 |
1.57 (0.85 – 2.91) |
0.140 |
|
Sex (Male) |
1.40 (0.82 – 2.41) |
0.220 |
130 (0.75 – 2.26) |
0.331 |
|
Co-morbidities |
|
|
|
|
|
Malignancy |
5 .77 (1.01 – 32.9) |
0.045 |
4 .90(0.89 -27.1) |
0 .067
|
|
Other comorbidities |
2 .36 (1.17 – 4.76) |
0.015 |
1.94 (0.92 – 4.11) |
0.082 |
|
Cause of sepsis |
|
|
|
|
|
Pneumonia |
0.78 (0.43 – 1.41) |
0.450 |
4.45 (1.02-19.45) |
1.000 |
|
UTI |
0.42 (0.15 – 1.17) |
0.960 |
2.37 (0.65 – 8.67) |
1.000 |
|
SBP |
4.53 (1.78 – 11.5) |
0.001 |
3.85 (1.43 -0.103) |
0.007 |
|
Blood stream infection |
4.19 (1.51 -11.6) |
0.002 |
3.62 (1.25 – 10.5) |
0.018 |
|
Skin infections |
5.67 (1.28 – 25.0) |
0.03 |
4.30 (0.95 – 19.3) |
0.059 |
|
Others (combined)* |
0.26 (0.07 – 0.95) |
0.411 |
1.52 (0.35 – 6.65) |
1.000 |
|
Culture reports |
|
|
||
|
Gram-negative bacteria |
0 .66 (0.22 – 2.01) |
0 .554 |
1.18 (0.29 – 4.08) |
0.816 |
|
Gram-positive bacteria |
1.04 (0.26- 4.08) |
1.000 |
0.85 (0.21 -3.44) |
1.000 |
|
Others** |
2.03 (0.48 – 8.48) |
3.900 |
2.10 (0.48 – 9.11) |
0.322 |
|
Intensive care treatment |
|
|
|
|
|
Intubation required |
29.66 (15.0 – 58.7) |
<0.001 |
23.5(11.2-49.2) |
<0.001 |
|
Pressors required |
12.27 (5.5 – 27.2) |
<0.001 |
9 .78 (4.02 – 23.8) |
<0.001 |
CI: confidence interval
SBP: Spontaneous bacterial peritonitis; UTI: Urinary tract infection.
*Others include tuberculosis, autoimmune diseases, scrub typhus, dengue, leptospirosis
**Others include tuberculosis, dengue, scrub typhus, leptospirosis, detected via Gene Xpert and serology tests
The microbiological culture profile in this study demonstrated a predominance of gram-negative organisms, with Escherichia coli (34.5%) and Klebsiella species (18.5%) being the most frequently isolated pathogens. This pattern aligns with findings from other South Asian countries, where gram-negative pathogens are frequently implicated in sepsis6,11,22. However, no statistically significant association was observed between culture positivity and mortality, which may be attributed to factors such as prior antibiotic use, low sensitivity of conventional culture methods, or delayed sample collection. Furthermore, a substantial proportion of sepsis cases were culture-negative, a phenomenon also documented in other studies, which poses challenges for targeted antimicrobial therapy23,24.
Pneumonia was the most common cause of sepsis (39.2%), followed by urinary tract infections (12.6%) and meningoencephalitis (9%). This finding aligns with studies from India, which reported respiratory infections as the most common source of sepsis (37.2%), followed by urinary tract infections (10.3%) and intra-abdominal infections (9.5%)13. Similarly, studies in the United States also identified pneumonia as the primary cause of sepsis and the leading contributor to mortality23. While pneumonia was the most frequent cause, spontaneous bacterial peritonitis (SBP) and bloodstream infections were significantly associated with higher mortality. These findings suggest that while pneumonia remains a key contributor to sepsis burden, intra-abdominal and hematogenous infections may carry a more severe clinical course, likely due to delayed diagnosis, multidrug-resistant pathogens, or rapid progression to organ failure. Patients with SBP are noted to have a higher progression rate to death or liver transplantation within one month compared to others25. Furthermore, patients with SBP due to extensively drug-resistant bacteria have a 30-day mortality rate of 69.2%26.
LIMITATIONS
This study has few limitations. Firstly, as single-centre study, the findings may not be generalizable to other healthcare settings in Bhutan. Secondly, the reliance on microbiological cultures may have underestimated pathogen prevalence, particularly in cases where antibiotics were administered prior to sample collection. Similarly, culture-negative sepsis also contributes to underestimating pathogen prevalence. Finally, small sample sizes for certain conditions like malignancy and specific infections may have reduced the power to detect statistically significant associations.
CONCLUSIONS
One-quarter of patients admitted with sepsis at the Department of Medicine at the JDWNRH had in-hospital mortality with significant associations observed for advanced age, SBP, bloodstream infections, and the need for mechanical ventilation and vasopressor support. To reduce the burden of sepsis and its associated mortality, national clinical guidelines on early recognition and timely administration of antibiotics must be developed. There is also a need to improve microbiological diagnostics, expand critical care capacity and train healthcare workers on sepsis management and enhance infection prevention strategies to improve outcomes.
ACKNOWLEDGEMENT
I would like to thank the staff of Department of Medicine for their support in carrying out the research. I also extend my gratitude to Dr. Tshokey, then microbiologist at JDWNRH.
REFERENCES
1. World Health Organisation. Global report on the epidemiology and burden of sepsis: current evidence, identifying gaps and future directions, 2020:14 [Full Text]
2. Angus DC, Van der Poll T. Severe sepsis and septic shock. N Engl J Med. 2013;369(9):840-51. [PubMed][Full Text] [DOI]
3. Novosad SA, Sapiano MRP, Grigg C, Lake J, Robyn M, Dumyati G, et al. Vital Signs: Epidemiology of Sepsis: Prevalence of Health Care Factors and Opportunities for Prevention. MMWR Morb Mortal Wkly Rep. 2016;65(33):864-9.[Full Text] [DOI]
4. Hammond NE, Kumar A, Kaur P, Tirupakuzhi Vijayaraghavan BK, Ghosh A, Grattan S, et al; Sepsis in India Prevalence Study (SIPS) Investigator Network. Estimates of Sepsis Prevalence and Outcomes in Adult Patients in the ICU in India: A Cross-sectional Study. Chest. 2022;161(6):1543-1554. [PubMed] [Full Text][DOI]
5. Lamichhane S, Manandhar N, Dhakal S, Shakya YL. Management and Outcome of Severe Sepsis and Septic Shock Patients. J Nepal Health Res Counc. 2018;16(2):165-171. [PubMed] [Full Text]
6. Kamal AHM, Karmaker P, Khatun W, Kumar Saha A, Rahman Md L, Hassan P, Management of Sepsis in Intensive Care Units in Rajshahi Medical College, Bangladesh. Adv Infect Dis. 2020;10:11-25. [Full Text] [DOI]
7. Jatsho J, Nishizawa Y, Pelzom D, Sharma R. Clinical and Bacteriological Profile of Neonatal Sepsis: A Prospective Hospital-Based Study. Int J Pediatr;2020:183 [PubMed] [Full Text] [DOI]
8. Bone RC, Balk RA, Cerra FB, Dellinger RP, Fein AM, Knaus WA, et al. Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. The ACCP/SCCM Consensus Conference Committee. American College of Chest Physicians/Society of Critical Care Medicine. Chest. 1992;101(6):1644-55. [Pub Med] [Full Text] [DOI]
9. Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA. 2016;315(8):801-10. [PubMed] [Full Text] [DOI]
10.Ministry of Health. Annual Health Bulletin 2018. Health Management and Information System, Policy and Planning Division, Ministry of Health, Royal Government of Bhutan, 2018;118p [Full Text]
11.Ahmed F, Faruq M, Ahsan A, Fatema K, Zaman S. Spectrum of Severe Sepsis in Critically Ill Adult Patients of Bangladesh: A Prospective Observational study. Bangladesh Crit Care J 2015;3:45–48. [Full Text] [DOI]
12.Ministry of Health. Annual Health Bulletin 2020, Health Management and Information System, Policy and Planning Division, Ministry of Health, Royal Government of Bhutan, 2020;144p. [Full Text]
13.Paary T T, Kalaiselvan M S, Renuka M K, Arunkumar A S. Clinical profile and outcome of patients with severe sepsis treated in an intensive care unit in India. Ceylon Med J. 2016;61(4):181-184. [PubMed] [Full Text] [DOI]
14.Todi S, Chatterjee S, Sahu S, Bhattacharyya M. Epidemiology of severe sepsis in India: an update. Crit Care. 2010;14(Suppl 1):382. [PubMed] [Full Text] [DOI]
15.Do SN, Luong CQ, Pham DT, Nguyen MH, Nguyen NT, Huynh DQ, et al. Factors relating to mortality in septic patients in Vietnamese intensive care units from a subgroup analysis of MOSAICS II study. Sci Rep. 2021;11(1):18924. [PubMed] [Full Text] [DOI]
16.Angstwurm MW, Gaertner R, Schopohl J. Outcome in elderly patients with severe infection is influenced by sex hormones but not gender. Crit Care Med. 2005;33(12):2786-93. [PubMed] [Full Text] [DOI]
17.Nasa P, Juneja D, Singh O, Dang R, Arora V. Severe sepsis and its impact on outcome in elderly and very elderly patients admitted in intensive care unit. J Intensive Care Med. 2012;27(3):179-83. [PubMed] [Full Text] [DOI]
18.Sakr Y, Jaschinski U, Wittebole X, Szakmany T, Lipman J, Ñamendys-Silva SA, et al. Sepsis in Intensive Care Unit Patients: Worldwide Data From the Intensive Care over Nations Audit. Open Forum Infect Dis. 2018;5(12):ofy313. [PubMed] [Full Text] [DOI]
19.Kang, C., Choi, S., Jang, E.J. et al. Prevalence and outcomes of chronic comorbid conditions in patients with sepsis in Korea: a nationwide cohort study from 2011 to 2016. BMC Infect Dis. 2024;24(1):184. [PubMed][DOI][Full Text]
20.Nachtigall I, Tafelski S, Rothbart A, Kaufner L, Schmidt M, Tamarkin A et al. Gender-related outcome difference is related to course of sepsis on mixed ICUs: a prospective, observational clinical study. Crit Care. 2011;15(3):R151. [PubMed] [Full Text] [DOI]
21.Li H, Pan X, Zhang S, Shen X, Li W, Shang W, et al. Association of autoimmune diseases with the occurrence and 28-day mortality of sepsis: an observational and Mendelian randomization study. Crit Care. 2023;27(1):476. [PubMed] [Full Text] [DOI]
22.Southeast Asia Infectious Disease Clinical Research Network. Causes and outcomes of sepsis in Southeast Asia: a multinational multicentre cross-sectional study. Lancet Glob Health. 2017;5(2):e157–67.[Full Text] [DOI]
23.Monti G, Landoni G, Taddeo D, Isella F, Zangrillo A. Clinical aspects of sepsis: an overview. Methods Mol Biol. 2015;1237:17-33[PubMed] [Full Text] [DOI]
24.Phua J, Ngerng W, See K, Tay C, Kiong T, Lim H, et al. Characteristics and outcomes of culture-negative versus culture-positive severe sepsis. Crit Care. 2013;17(5). [PubMed] [Full Text] [DOI]
25.Furey C, Zhou S, Park JH, Foong A, Chowdhury A, Dawit L, et al. Impact of Bacteria Types on the Clinical Outcomes of Spontaneous Bacterial Peritonitis. Dig Dis Sci. 2023;68(5):2140-48. [PubMed] [Full Text] [DOI]
26.Alexopoulou A, Vasilieva L, Agiasotelli D, Siranidi K, Pouriki S, Tsiriga A, et all. Extensively drug-resistant bacteria are an independent predictive factor of mortality in 130 patients with spontaneous bacterial peritonitis or spontaneous bacteremia. World J Gastroenterol. 2016;22(15):4049-56. [PubMed] [Full Text] [DOI]