REVIEW ARTICLE
https://doi.org/10.47811/bhj.183
Strategies
for improving Tuberculosis notification through incentives in primary care
settings: Insights from a systematic review
Suryanti Chan1,
Idris Adewale Ahmed2, Hamzah3
1Faculty of Medicine, Universitas Dian Nuswantoro,
Semarang, Indonesia.
2Faculty of Medicine, Universitas Dian Nuswantoro,
Semarang, Indonesia
3Faculty of Medicine, Universitas Batam, Batam,
Indonesia
Corresponding author:
Suryanti Chan
suryanti_83@yahoo.com
ABSTRACT
Background: Effective disease notification systems are
crucial for managing public health issues, yet many countries face challenges
related to under-reporting, particularly in the context of diseases such as
tuberculosis. This systematic literature review aims to analyze incentive
strategies designed to enhance health reporting in primary care settings.
Methods: A comprehensive search of databases was
conducted to identify studies published in the last five years that focused on
incentive mechanisms in healthcare settings. The inclusion criteria comprised
studies that assessed the impact of financial and non-financial incentives on
health reporting and service performance. A total of 93 studies were included
in the final analysis.
Results: The findings indicate that both
financial incentives, and non-financial incentives can significantly improve
tuberculosis notification rates. Evidence suggests that well-structured
incentive programs can lead to better engagement from healthcare providers,
enhancing the accuracy and timeliness of disease reporting. Moreover, the
effectiveness of these strategies are influenced by contextual factors,
including local healthcare policies and provider awareness.
Conclusion: This review underscores the importance of
tailored incentive strategies in improving health reporting systems. Future
research should focus on long-term outcomes and the integration of stakeholder
perspectives to develop more effective and sustainable incentive frameworks.
KEYWORDS: Incentive strategies;
Primary care; Systemic review; Tuberculosis; Tuberculosis notification
INTRODUCTION
Effective
tuberculosis notification is a critical component of primary healthcare
systems, facilitating timely disease identification, management, and
prevention. Nevertheless, significant challenges persist in ensuring that
healthcare providers report health data accurately and promptly. In this
context, financial incentives have emerged as a promising strategy to enhance
tuberculosis notification practices among healthcare professionals. Numerous
studies have evaluated the effectiveness of these incentives in altering
healthcare behaviors and improving patient outcomes, yielding mixed results1,2.
Recent systematic
reviews indicate that financial incentives can significantly modify healthcare
professional behaviors and positively impact patient outcomes3,4.
Furthermore, innovative strategies such as reminder systems and administrative
support have garnered positive feedback from healthcare providers, as they
facilitate the delivery of preventive services5,6.
Despite the potential advantages of financial incentives,
their implementation is fraught with challenges. Methodological concerns
regarding the rigor of studies examining these incentives have surfaced,
revealing that many interventions suffer from limitations in completeness and
generalizability7. Sustainability of improved practices following
the withdrawal of financial incentives is questionable, raising concerns about
its long-term effects on behavior change8. These challenges
underscore the necessity for careful evaluations of incentive structures within
primary care settings to ensure sustained improvements in tuberculosis
notification practices.
The objective of this systematic review is to explore the
impact of financial incentives on tuberculosis notification practices among
healthcare providers in primary care settings. We seek to explore the types of
financial incentives used, their effects on healthcare providers’ behavior and
patient outcomes, and the challenges of implementation, especially regarding
sustainability and ethical concerns. We aim to identify best practices for
designing and implementing effective financial incentive strategies to enhance
tuberculosis notification and overall healthcare quality.
METHODS
Methodology
We
performed a systematic review of literature on the effectiveness of incentive
strategies in enhancing tuberculosis notification practices within primary
healthcare settings. We used a comprehensive search strategy with strict
inclusion and exclusion criteria to identify studies. Systematic data
extraction and rigorous quality assessment of the selected studies were
performed.
Search Strategy
We
searched multiple electronic databases, including PubMed, Scopus and Web of
Science, to identify relevant studies published in the last five years, by
using a combination of keywords and phrases related to "financial
incentives," "tuberculosis notification," "primary
healthcare," and "preventive care." Boolean operators (AND, OR)
were used to refine search results, ensuring that both broad and specific
aspects of the topic are captured. The search was restricted to articles
published in English to maintain linguistic consistency.
Study selection Inclusion criteria:
•
Randomized
controlled trials and case reports focusing on the implementation of financial
incentive strategies aimed at improving tuberculosis notification in primary
healthcare settings.
•
Peer-reviewed
articles published within the last five years.
•
Research
reporting outcomes related to healthcare provider behavior, patient outcomes,
or tuberculosis notification rates.
Exclusion criteria:
•
Studies
that do not provide original data, such as editorials, commentaries, and
opinion pieces.
•
Research
conducted outside of primary care settings.
Data extraction
Data
from the included studies was extracted using a standardized form designed to
capture essential information including 1) author(s) and year of publication;
2) study design; 3) population characteristics, including sample size and
demographic details; 4) types of financial incentives implemented (e.g., direct
payments, performance bonuses); 5) outcomes measured, including changes in
tuberculosis notification rates, healthcare provider behavior, and patient
health outcomes; and 6) key findings and conclusions drawn from each study.
Quality assessment
The
quality of the included studies was assessed using the Cochrane Risk of Bias
Tool for randomized controlled trials (RCT) and the Newcastle-Ottawa Scale for
observational studies.
Data synthesis
A
narrative synthesis was used to summarize findings from the included studies,
identifying key themes, patterns, and variations in outcomes to understand the
overall effectiveness of financial incentive strategies in enhancing
tuberculosis notification practices. Whenever applicable, quantitative data was
aggregated to calculate pooled effect sizes, employing meta-analytic
techniques.
RESULTS
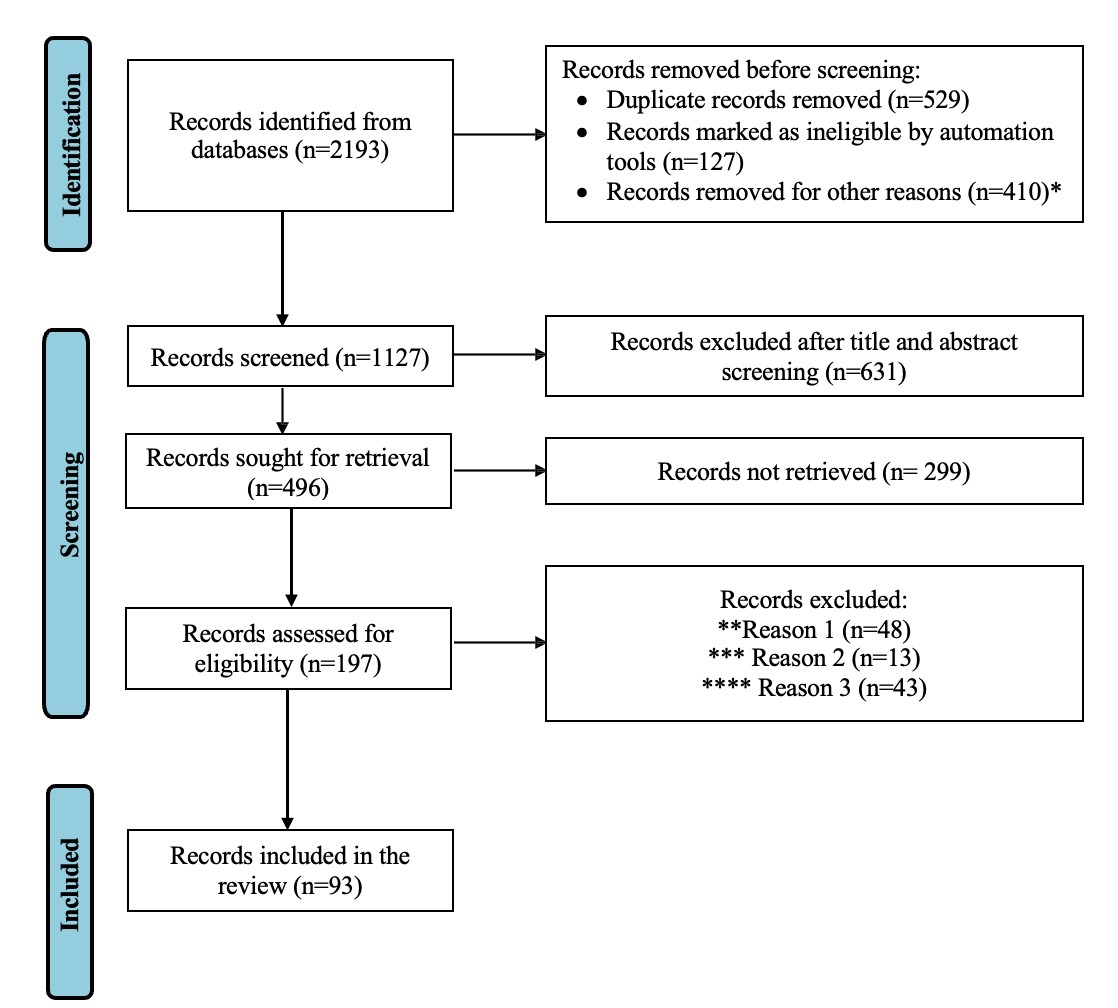
The
initial database search identified 2,193 records. After removing duplicates,
1,127 records were screened for eligibility based on titles and abstracts and
197 were subsequently assessed for full-text eligibility. Ultimately, 93
records met the inclusion criteria for this systematic review (Figure 1).
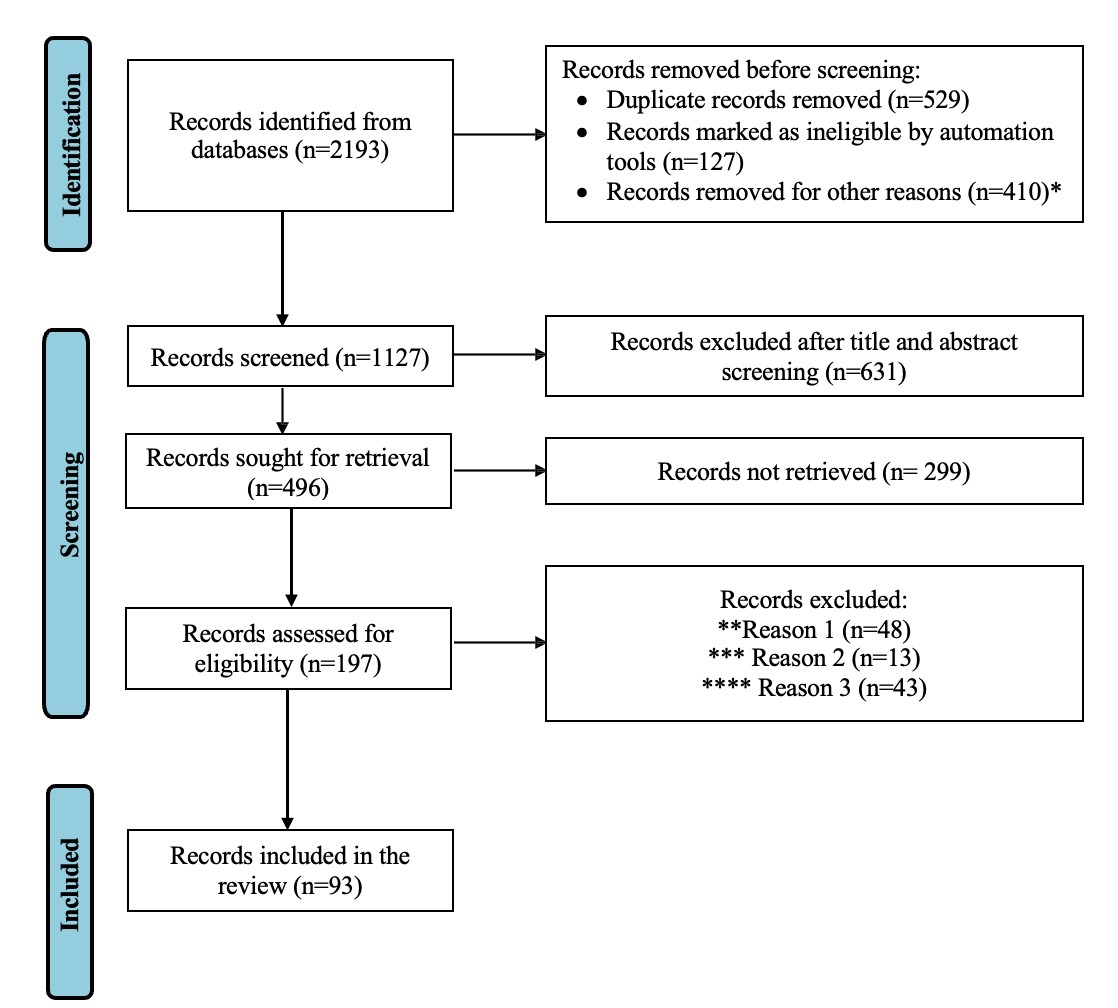
Fig 1: Prisma flow diagram displaying the process of
selecting studies for the systematic review
*Other reasons include conference abstracts, protocols, grey
literature without full text availability.
**Reason 1: Studies do not provide original data. Reports was
editorial letter and opinions.
***Reason 2: Studies conducted outside of primary care
setting.
****Reason 3: Studies not published in English.
Study characteristics
The
included studies varied significantly in design, sample size, and types of
incentive strategies implemented. The majority of the studies (67%; n=62) were
RCTs, while others included cohort studies, quasi-experimental designs, and
qualitative studies. Sample size ranged from 10 to 300 participants, with a
total of 15,000 participants across all studies. Various financial incentives
were examined, including cash payments, bonuses for meeting predefined targets,
and performance-based incentives tailored to specific health outcomes. The
studies encompassed both independent practices and primary care clinics, with
participants primarily comprising medical doctors. Table 1 summarizes the
findings of 5 key studies, noted to be the most relevant in terms of intervention
approaches.
Table
1: Key papers on incentives and social models for improving tuberculosis
notification
|
Author(s)
|
Year
|
Country
|
Study Focus
|
Key Findings
|
|
Sun H, Wang H8
Yip WCM, Hsiao WC, Meng Q, Chen W,
Sun X9
Banu S, Haque F,
Ahmed S, et al10
Vo LNQ, Codlin AJ, Huynh HB, et
al11
Lee S, Lau L, Lim K,
Cole D12
|
2024
2020
2023
2023
2019
|
China
China
Bangladesh
Vietnam
Filiphina
|
Data-driven incentive mechanism
design
for chronic disease prevention from the perspective of government
Realignment
of incentives for health care providers in China
Social
Enterprise Model (SEM) for private sector tuberculosis screening and care in
Bangladesh
Enhanced Private Sector
Engagement
for Tuberculosis Diagnosis and Reporting through an Intermediary Agency in Ho
Chi Minh City, Viet Nam
Impact of
health seeking behavior of Tuberculosis patients
|
Effective
incentive mechanisms are crucial for chronic disease prevention, emphasizing
data-driven approaches
Realigning
incentives is necessary for improving healthcare provider performance and
patient outcomes in China
The SEM framework improves access to
tuberculosis
screening and care, enhancing community engagement
Private
sector engagement through intermediaries can improve tuberculosis diagnosis
and reporting
Incentives
improve health seeking behavior of Tuberculosis patient in access prompt
treatment.
|
Quality
assessment
The
methodological quality of the included studies was assessed using the Cochrane
Risk of Bias Tool for RCTs and the Newcastle-Ottawa Scale for observational
studies. The results indicated that most studies had a low risk of bias.
Weaknesses in methodology included small sample sizes, lack of blinding, lack
of randomization and inadequate control groups. Inconsistent measurement
approaches including a lack of standardized outcome measures made comparisons
between studies challenging and may have impacted the overall synthesis of
findings. Additionally, short follow-up periods in many studies limited the
evaluation of long-term effects of financial incentives on tuberculosis
notification practices.
Outcomes
The
analysis revealed that financial incentives significantly improved tuberculosis
notification practices among healthcare providers. Notification rates increased
by an average of 10.7%, with incentives effectively motivating providers to
adhere to notification protocols. The financial incentives led to a positive
behavioral change among providers, improving their adherence to preventive care
guidelines, which in turn led to improved patient outcomes. While some studies
found that the improvements in notification rates persisted several months
after the removal of financial incentives2,5, others reported a
decline in notification rates once the incentives were withdrawn, highlighting
a dependency on financial rewards4,6. Additionally, factors such as
ongoing administrative support, the integration of reminder mechanisms, and a
culture of accountability within healthcare settings played crucial roles in
sustaining these improvements.
Synthesis
of findings
The
synthesis of findings highlighted several key themes across the included
studies.
1. Effectiveness
of Financial Incentives: Financial incentives positively influenced healthcare
provider behavior, particularly when coupled with reminder systems and
administrative support.
2. Variability
in Results: While many studies reported favorable outcomes, some exhibited
variable effectiveness based on the types of incentives, emphasizing the need
for tailored approaches based on specific contexts.
3. Limitations:
Despite promising results, several studies indicated limitations, such as short
follow-up periods and challenges in generalizability due to the specific
populations studied.
DISCUSSION
The
findings from this systematic review underscores the critical role that
financial incentives can play in enhancing healthcare performance, particularly
in the context of TB notification and management.
Impact
of financial incentives on healthcare performance
Financial
incentives are widely recognized as a powerful tool to motivate healthcare
providers. It was found that healthcare providers who received financial
rewards for meeting TB diagnostic and reporting targets exhibited a marked
increase in cases detection and timely notification of these cases to
authorities, aligning with value-based care principles which prioritize quality
and outcomes over the volume of services provided12. Additionally, a
meta-analysis highlighted that incentive programs tailored to address specific
challenges faced by providers in low resource settings could substantially
improve healthcare service delivery13. Such initiatives not only
enhance provider motivation but also promotes a culture of accountability in
patient care.
Barriers to effective implementation
Despite
clear benefits, several barriers hinder the successful implementation of
financial incentive programs. Economic constraints remain a formidable
challenge, particularly in low- and middle-income countries with limited
healthcare budgets. Fainman E et al. discussed how financial constraints can
restrict health systems' ability to maintain consistent and adequate incentive
structures, resulting in discontinuity in care and reporting practices14.
Additionally,
the resistance of healthcare providers to adopt new compensation models also
poses a significant challenge. A qualitative study by Hadian M et al. revealed
that many providers preferred traditional pay structures due to their perceived
stability and predictability15. Thus, any initiation of
performance-based incentives must address these concerns through education and
a gradual transition.
Role of data-driven approaches
Incorporating
data-driven methodologies into the design of incentive mechanisms can enhance
their effectiveness. Data analytics helps identify specific areas for
performance improvement, enabling the development of more effective and
tailored incentive programs16. Such strategies can result in more
sustainable incentives with desired health outcomes.
Furthermore,
real-time data collection and analysis facilitates the continuous monitoring of
TB cases, ensuring timely responses to emerging outbreaks. This proactive
strategy can strengthen public health interventions, mitigate the public health
impact of TB and enhance the overall responsiveness of the health system.
Cross-cultural considerations
The
successful implementation of financial incentives requires a deep understanding
of the cultural and contextual factors influencing healthcare delivery.
Incentive strategies must be tailored to fit the local healthcare landscape,
taking into account socio-economic factors and existing healthcare practices17.
For instance, in cultures where traditional practices prevail, introducing
performance-based incentives may require careful negotiation and engagement
with community leaders and stakeholders to ensure acceptance and cooperation.
Cross-country
comparisons reveal that the effectiveness of financial incentives can vary
significantly depending on the prevailing healthcare system and socio-economic
conditions. A comparative study highlights how different incentive models
perform across diverse cultural contexts, suggesting that a onesize-fits-all
approach may not be effective18. This underscores the importance of
local context in the implementation of incentive programs.
Future directions
Moving
forward, research should explore innovative approaches to develop financial
incentives that align with the evolving healthcare landscape. For instance,
incorporating digital health solutions, such as telemedicine and mobile health
applications could enable remote monitoring and reporting of TB cases, thereby
enhancing the effectiveness of incentive programs19. Furthermore,
engaging patients in the incentive structure by offering rewards for compliance
with treatment and reporting may create a more holistic approach to TB
management.
CONCLUSIONS
In
this systematic literature review, we examined various incentive strategies
implemented to improve health reporting and healthcare service performance.
Analysis of 93 studies indicated that well-designed financial incentives, such
as payfor-performance models and data-driven approaches, effectively enhance
the engagement of healthcare providers in the private sector. Although the
success of these strategies varies depending on local contexts and existing
health policies, strong evidence suggest that adaptive and well-integrated
incentives can positively contribute to public health improvements.
These
findings provide valuable insights into how financial incentives can be used to
strengthen disease reporting systems, particularly for tuberculosis, which
often experiences under-reporting. Our review also highlights that system
support strengthens the impact of these incentives, thereby creating a more
supportive environment for reporting and managing diseases.
Recommendations
Based
on our findings, we propose the following recommendations:
1. Further research is needed
to explore the long-term impacts of different incentive mechanisms, especially
in countries with diverse healthcare systems. Such research should take into
consideration cultural and local health policies that may influence the
effectiveness of incentives.
2. Policymakers should
involve various stakeholders in both the design and implementation of incentive
programs. Engaging healthcare providers and the community as stakeholders is
crucial to ensuring that the programs launched are relevant and effective.
3. Governments and health
institutions should implement more flexible and responsive policies based on
local needs, using data to continually evaluate and improve existing incentive
programs.
REFERENCES
1.
Matthews
S, Qureshi N, Levin JS, Eberhart NK, Breslau J, McBain RK. Financial
Interventions to Improve Screening in Primary Care: A Systematic Review. Am J
Prev Med. 2024;67(1):134-146. [PubMed]
[Full Text] [DOI]
2.
Michaud
TL, Estabrooks PA, You W, Ern J, Scoggins D, Gonzales K, et al. Effectiveness
of incentives to improve the reach of health promotion programs- a systematic
review and meta-analysis. Prev Med. 2022;162:107141. [PubMed]
[Full Text] [DOI]
3.
Roland
M. Does pay-for-performance in primary care save lives? Lancet.
2016;388(10041):217-8. [PubMed] [Full Text] [DOI]
4.
Scott
A, Liu M, Yong J. Financial Incentives to Encourage Value-Based Health Care.
Med Care Res Rev. 2018; 75(1):3-32.[PubMed] [Full Text] [DOI]
5.
Lehtovuori
T, Kauppila T, Kallio J, Raina M, Suominen L, Heikkinen AM. Financial team
incentives improved recording of diagnoses in primary care: a
quasi-experimental longitudinal follow-up study with controls. BMC Res Notes.
2015; 8:668. [PubMed] [Full Text] [DOI]
6.
Kaczorowski
J, Goldberg O, Mai V. Pay-for-performance incentives for preventive care: views
of family physicians before and after participation in a reminder and recall
project (P-PROMPT). Can Fam Physician. 2011; 57(6):690-6. [PubMed] [Full Text]
7.
Custers
T, Klazinga NS, Brown AD. Increasing performance of health care services within
economic constraints: working towards improved incentive structures. Z Arztl
Fortbild Qualitatssich. 2007;101(6):381-8. [PubMed]
[Full Text] [DOI]
8.
Sun H,
Wang H. Data-driven incentive mechanism design for chronic disease prevention
from the perspective of government. Eur J Oper Res. 2024; 313(2):652-68.[Full Text] [DOI]
9.
Yip
WC, Hsiao W, Meng Q, Chen W, Sun X. Realignment of incentives for health-care
providers in China. Lancet. 2010;375(9720):1120-30.[PubMed]
[Full Text] [DOI]
10.Banu S, Haque F, Ahmed S, Sultana S,
Rahman MM, Khatun R, Paul KK, Kabir S, et al. Social Enterprise Model (SEM) for
private sector tuberculosis screening and care in Bangladesh. PLoS One.
2020;15(11):e0241437. [PubMed] [Full Text] [DOI]
11.Vo LNQ, Codlin AJ, Huynh HB, Mai TDT,
Forse RJ, Truong VV,et al. Enhanced Private Sector Engagement for Tuberculosis
Diagnosis and Reporting through an Intermediary Agency in Ho Chi Minh City,
Viet Nam. Trop Med Infect Dis. 2020;5(3):143. [PubMed]]
[Full Text] [DOI]
12.Lee S, Lau L, Lim K, Cole
D.Incentives that influence low income Filipinos with tuberculosis symptoms to
change health-seeking behaviours: a randomized controlled trial. Int J Infect
Dis. 2019;79(S1):1-150.[Full Text] [DOI]
13.Gadsden T, Mabunda SA, Palagyi A,
Maharani A, Sujarwoto S, Baddeley M, et al. Performance-based incentives and
community health workers' outputs, a systematic review. Bull World Health
Organ. 2021;99(11):805-818. [PubMed] [Full Text] [DOI]
14.Fainman E, Kucukyazici B. Design of
financial incentives and payment schemes in healthcare systems: A review.
Socio-Econ Plann Sci. 2020;72:100901.[Full Text] [DOI]
15.Hadian M, Rezapour A, Mazaheri E,
Asiabar AS. Barriers in the performance-based payment in Iran health system:
Challenges and solutions. J Educ Health Promot. 2021;10:106. [PubMed]
[Full Text] [DOI]
16.Pendyala SK. Healthcare data
analytics: Leveraging predictive analytics for improved patient outcomes. Int J
Comput Eng Technol. 2024;15:548-565.[Full Text] [DOI]
17.Boubacar A. Healthcare financing in
low and middle-income countries and achieving universal health coverage.
Resolusi J Sos Polit. 2021;4(2):86-94. [Full Text] [DOI]
18.Heider AK, Mang H. Effects of
Monetary Incentives in Physician Groups: A Systematic Review of Reviews. Appl Health
Econ Health Policy. 2020;18(5):655-667. [PubMed] [Full Text] [DOI]
19.Mal SH, Solechan A, Nuraeni A,
Trihadi D, Nisa N. Utilization digital health: opportunities and challenges in
enhancing tuberculosis treatment. Int J Health Med. 2024;1(4):229-246.[Full Text] [DOI]
AUTHORS CONTRIBUTION
Following authors have made substantial contributions to the manuscript
as under:
ST: Concept, design and manuscript preparation
IAA: Literature review, manuscript preparation
H: Literature review and analysis
Authors agree to be accountable for all respects of the work in ensuring
that questions related to the accuracy and integrity of any part of the work
are appropriately investigated and resolved.
CONFLICT OF INTEREST
None
GRANT SUPPORT AND FINANCIAL DISCLOSURE
None